What is Semaglutide
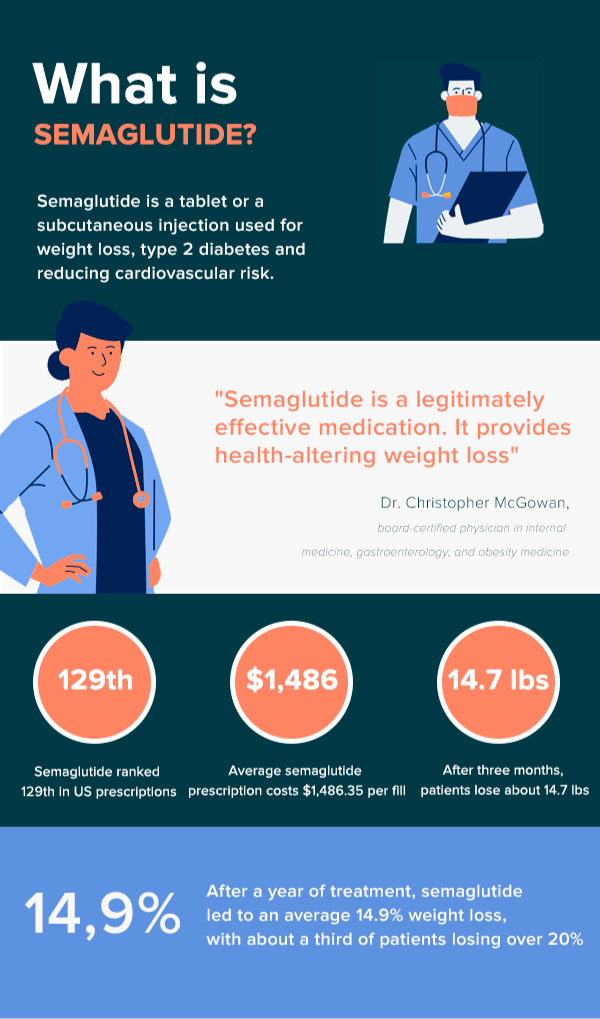
Semaglutide is a medication used primarily to treat type 2 diabetes and to assist in weight management. Classified as a GLP-1 receptor agonist, it mimics the functions of an incretin hormone, glucagon-like peptide-1 (GLP-1), which is naturally produced in the body and plays a vital role in the regulation of blood sugar levels. Semaglutide works by stimulating the pancreas to release insulin more effectively, especially when blood sugar levels are high. It also reduces the amount of glucagon being produced. Glucagon is a hormone that works opposite to insulin, raising blood sugar levels, so its reduction is beneficial in managing diabetes.
Another key aspect of semaglutide is its ability to slow down the movement of food through the stomach. This results in patients feeling fuller for longer periods, thus reducing their overall food intake. Consequently, semaglutide has become increasingly popular for its weight loss benefits. In addition to its effects on blood sugar and weight, semaglutide is also known for its cardiovascular benefits, making it a comprehensive treatment option for individuals with type 2 diabetes, particularly those who are overweight or struggle with obesity. Administered via injection or orally, semaglutide is an important part of modern diabetes management and weight loss strategies.
While semaglutide is effective and has transformed the management of type 2 diabetes and weight loss, it is important for patients to consult healthcare professionals before starting the treatment, as it may not be suitable for everyone and can have side effects such as gastrointestinal discomfort. Regular monitoring and adherence to the prescribed regimen are crucial for achieving the best results with semaglutide.
Current researches about Semaglutide
Semaglutide 2.4 mg for weight loss in adults with overweight or obesity
The phase III STEP clinical program has made significant strides in the field of obesity treatment, highlighting that a 2.4 mg semaglutide dosage offers clinically meaningful and lasting weight loss, surpassing results from other available obesity agents. The study underscores the positive impact of semaglutide for weight loss, not just in shedding pounds but also in enhancing the quality of life and health of individuals with obesity or overweight, with or without type 2 diabetes (T2D).
Remarkably, the research revealed that semaglutide could facilitate double-digit weight loss, which is linked to the potential remission of T2D. This finding is particularly groundbreaking as it shifts the treatment paradigm from focusing primarily on glucose control to a more weight-centric approach. With semaglutide for weight loss in 2.4 ml dosage, achieving ambitious weight loss goals is now within reach, prompting a reevaluation of current T2D treatment strategies.
Furthermore, the use of once-weekly semaglutide for weight loss in nondiabetics is poised to become an integral component in treating individuals with obesity or overweight, irrespective of their T2D status. This is largely due to its ability to address the pathological connection between obesity and T2D directly. Semaglutide doesn't just aid in weight reduction; it also has the potential to improve or even prevent complications associated with T2D. Additionally, it can alleviate numerous physical and mental health issues that often accompany obesity, making it a multifaceted tool in the fight against obesity-related health challenges.
Weight loss outcomes associated with semaglutide treatment for patients with overweight or obesity
The utilization of semaglutide for weight loss has demonstrated promising outcomes, especially for patients with overweight or obesity. In a real-world clinical setting, the effects of semaglutide treatment have mirrored the impressive weight loss results seen in randomized clinical trials. This correlation strongly suggests the practical applicability and effectiveness of semaglutide in treating individuals struggling with weight issues.
In a detailed cohort study involving 175 patients with overweight or obesity, the impact of semaglutide on weight reduction was closely monitored. The results were noteworthy: patients experienced an average total body weight loss of 5.9% at the 3-month mark and an even more significant 10.9% at 6 months. These percentages are indicative of semaglutide’s potent capability to aid weight loss over a relatively short period. The consistency of these results, aligning with those from controlled clinical trials, highlights semaglutide as a viable and potent option for those seeking medical assistance in their weight loss journey.
Once-weekly semaglutide in adolescents with obesity
In a comprehensive study involving 201 adolescents, most of whom were battling obesity, the effectiveness of semaglutide was put to the test. Out of all participants, an impressive 90% adhered to the treatment regimen until its completion. The treatment plan was distinctive, combining a once-weekly 2.4-mg dosage of semaglutide with targeted lifestyle interventions aimed at fostering healthier habits. Over the course of 68 weeks, the results were striking. Those in the semaglutide group witnessed a significant decrease in BMI, averaging a notable reduction of − 16.1%. This was in stark contrast to the placebo group, which only recorded a minimal change of 0.6%. The difference between the two groups was substantial, highlighting the efficacy of semaglutide in this context.
But the benefits of semaglutide went beyond mere weight loss. The study also found that adolescents receiving semaglutide experienced greater improvements in various cardiometabolic risk factors compared to their counterparts in the placebo group.These findings illuminate the promise of semaglutide for weight loss and health improvement in adolescents with obesity. The combination of semaglutide with lifestyle changes emerged as a potent approach, offering a viable and effective pathway for managing adolescent obesity and its associated health risks.